Table of Contents
Introduction
With trillions of nerves that are inhibiting the body, the nervous system is consist of the central nervous system and the peripheral nervous system, and its job is to make sure that the neuron signals are traveling to and fro from the brain to the entire body. When there is an unwanted pathogen that enters the body and starts to disrupt the neuron signals, it can cause a variety of neurodegenerative disorders and neuropathic problems to affect the body over time. In this 2 part series, we will be taking a look at what is neuropathic pain and its symptoms. In Part 1, we discussed and understand what is polyneuropathy and how different polyneuropathies can affect the body. By referring patients to qualified and skilled providers who specialized in neurological services. To that end, and when appropriate, we advise our patients to refer to our associated medical providers based on their examination. We find that education is the key to asking valuable questions to our providers. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer
Can my insurance cover it? Yes, in case you are uncertain here is the link to all the insurance providers we cover. If you have any questions, please call Dr. Jimenez at 915-850-0900.
What Is Neuropathic Pain?
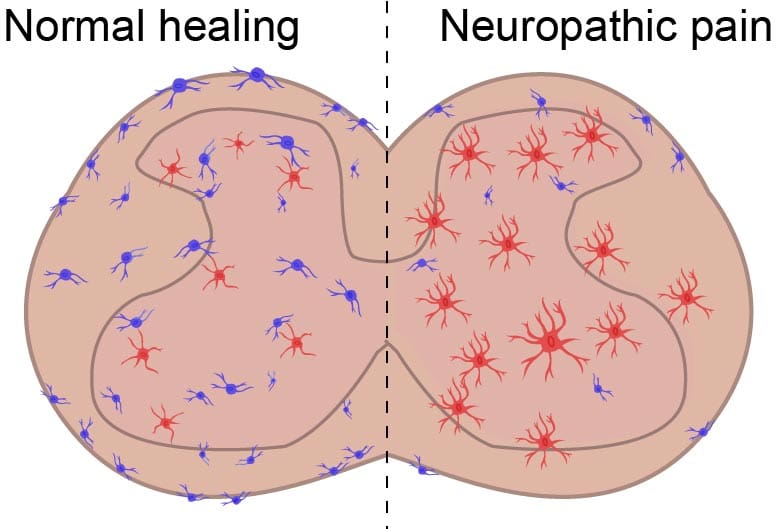
When there is pain that is radiating from the nerves, the spinal cord, or the brain, it is known as neuropathic pain. This type of pain doesn’t originate in the bones, muscles, or organs but is a direct consequence of diseases that is affecting the somatosensory system. Research studies have shown that neuropathic pain is caused by various central and peripheral nerve disorders that cause lesions in the nervous system. This can be problematic for individuals who have neuropathic pain because it can cause the body to appear normal but can be experienced in other parts of the body. Other research studies have found that neuropathic pain can cause mild to severe pain symptoms that can distort existing neuron signals, create new ones, or even prevent the neuron signals from transferring throughout the entire body.
The Symptoms
Since neuropathic pain in the body is chronic and is due to damaged nerves, research shows that even though neuropathic pain is a chronic progressive nerve disorder that can occur from injuries or infections that affect the body, it can send unprompted signals to the brain causing it to be dysfunctional. Other symptoms that neuropathic pain can cause to the body include:
- Numbness
- Burning pain
- Sleep difficulty
- Hypoalgesia
- Allodynia( cold pain)
- Metabolic disorders
- Inflammatory disorders
HCTP Therapy
As a form of regenerative treatment, stem cells* or HCTP (human cellular tissue products) can help boost the body’s own natural healing process by repairing and regenerating cells, damaged tissues, and diseased organs. HCTP is used in both international and nationally affiliated clinics and distribution organizations to help individuals that are in chronic pain and need relief. With more and upcoming research discovering beneficial properties of HCTP, many individuals can start living life to the fullest pain-free.
Small Fiber Polyneuropathy
Small fiber neuropathies (SFN) are a result of damage to the peripheral nerves affecting small myelinated A-delta and unmyelinated C fibers in the body. The fibers affected include both small somatic as well as autonomic fibers as they can be subserved through thermal perception and nociception by small fibers. With the enteric function is also subserved by small fibers, research shows that SFN is affected by the damaged peripheral nervous system causing the small fibers to cause burning pain or a tingle sensation on the feet and progress through the leg and throughout the entire body.
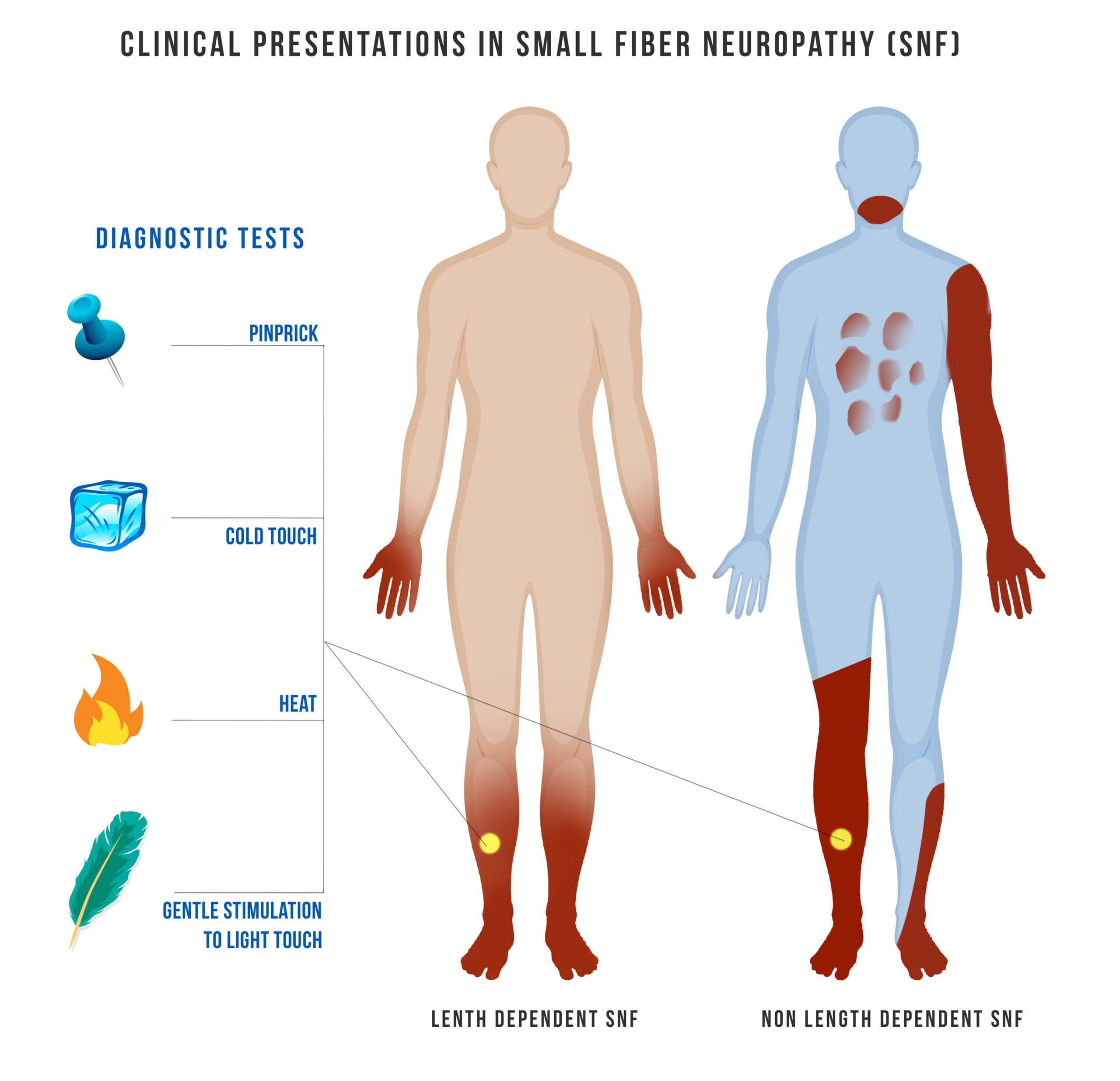
The pathogenesis of injury to small fibers is not well understood but when SFN starts to progress, it can involve the large fibers in the body. The large fibers are heavily myelinated and involved in muscle control, as well as touch, vibration, and position sense. So when SFN starts to affect the large fibers, it can cause muscle cramps on the body causing a person to be in pain unless it is treated. Other less common symptoms that SFN can be a result on the body involved the face, trunk, proximal limbs, or other more localized areas.
Small Fiber Polyneuropathy Symptoms
Some of the symptoms vary widely in severity when an individual is dealing with small fiber polyneuropathy as it is often affected to individuals that describes it as a gradual onset of vague distal sensory disturbances. Some of the examples include feeling like there is sand in the person’s shoe, a sock feeling as if it has pebbles in it, pins and needle sensations, cold painful sensations, or tingling. Other symptoms from SFN can include burning pain in the extremities and sometimes can be severe. Studies have found that some of the known causes of SFN can include diabetes Mellitus, amyloidosis, toxins, and inherited neuropathies. Other symptoms that are caused by SFN include:
- Allodynia and hyperesthesia
- Dry eyes and mouth
- Lightheadedness with changes in posture
- Syncope
- Abnormalities of sweating
- Erectile dysfunction
- GI symptoms (nausea and emesis, constipation, diarrhea, changes in urinary frequency including nocturia)
Conclusion
All in all, the nervous system’s primary function is to make sure that all the neuron signals are coming from the brain and traveling throughout the entire body while keeping a bidirectional communication with the brain. When unwanted pathogens like neuropathic pain and SFN are causing a disruption to the neuron signals, it can cause the body to be dysfunctional while causing pain to the individual. The individual will feel a tingling sensation or burning pain depending on how severe the neuropathic pain is. By making small changes that can help minimize chronic pain flare-ups like acupuncture or eating anti-inflammatory foods, individuals can get their lives back together pain-free.
References
Eske, Jamie. “Small Fiber Neuropathy: Symptoms, Treatment, Causes, and Progression.” Medical News Today, MediLexicon International, 2 Dec. 2021, www.medicalnewstoday.com/articles/small-fiber-neuropathy.
Gilron, Ian, et al. “Neuropathic Pain: A Practical Guide for the Clinician.” CMAJ : Canadian Medical Association Journal = Journal De L’Association Medicale Canadienne, Canadian Medical Association, 1 Aug. 2006, www.ncbi.nlm.nih.gov/pmc/articles/PMC1513412/.
Holland, Kimberly. “What You Should Know about Neuropathic Pain.” Healthline, Healthline Media, 5 Feb. 2020, www.healthline.com/health/neuropathic-pain.
Lacomis, David. “Small-Fiber Neuropathy.” Muscle & Nerve, U.S. National Library of Medicine, Aug. 2002, pubmed.ncbi.nlm.nih.gov/12210380/.
Sissons, Beth. “Neuropathic Pain: Causes, Types, and Treatment.” Medical News Today, MediLexicon International, 10 Feb. 2022, www.medicalnewstoday.com/articles/neuropathic-pain.
Disclaimer
General Disclaimer
Professional Scope of Practice *
The information herein on "A Look Into Neuropathic Pain | Part 2" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Welcome to El Paso's Premier Wellness and Injury Care Clinic & wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card