Table of Contents
Introduction
The gut system makes sure that any food that is being digested gets turned into nutrient particles and is transported all over the entire body. The food particles will be secreted out of the body to prevent waste from building up in the gut. The primary function of the gut system is to make sure that any food is being transformed into nutrients to help with growth, metabolism, and immune support for a functional body. The gut system also has a bidirectional connection to the brain as they send information back and forth to each other and keep the organs from being dysfunctional. When harmful pathogens enter the gut system, they can develop into chronic issues and affect the gut and the body. In this article, we will be looking at what GERD is, its symptoms, and how it can affect stomach acid. By referring patients to qualified and skilled providers who specialize in gastroenterology services. To that end, and when appropriate, we advise our patients to refer to our associated medical providers based on their examination. We find that education is the key to asking valuable questions to our providers. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer
Can my insurance cover it? Yes, it may. If you are uncertain, here is the link to all the insurance providers we cover. If you have any questions, please call Dr. Jimenez at 915-850-0900.
What Is GERD?
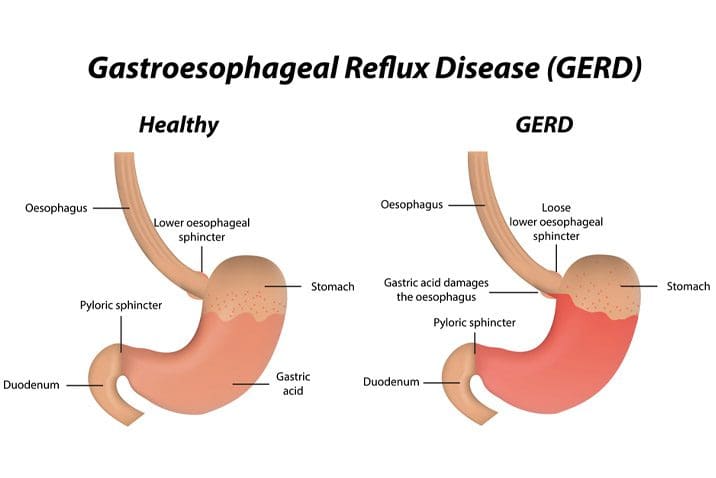
Research studies have shown that GERD usually occurs when stomach acid frequently flows back and forth in the tube, where the mouth and the esophagus are connected, irritating the esophagus wall lining. So GERD or gastroesophageal reflux disease is the reflux of gastric contents into the esophagus in normal physiology and is defined as reflux leading to symptoms, esophageal mucosal injury, or both. The majority of individuals with GERD will show no abnormalities on upper endoscopy, and there are not any esophageal lesions (erosions, ulceration, intestinal metaplasia) for them to be diagnosed with GERD. Other research studies have also shown that GERD is a common digestive disorder that affects people worldwide and has troublesome symptoms and conditions that can affect a person’s quality of life.
The Symptoms Of GERD
Some of the typical symptoms of GERD that individuals will experience are heartburn, which is painful retrosternal burning or pressure sensation that may be angina?like in quality, and regurgitation, which is the rising of gastric contents into the upper throat or mouth. Studies have shown that GERD can also be defined as mucosal damage due to the production of abnormal reflux of gastric contents. GERD can also be classified as NERD (non-erosive reflux disease) or ERD (erosive reflux disease) depending on how severe the presence or absence of esophageal mucosal damage GERD has caused in the esophagus. Some of the other symptoms that GERD can cause to the gut system and the body include:
- Hoarseness
- Cough
- Asthma
- Pharyngitis
- Erosion of dental enamel
- Sinusitis
- Pulmonary fibrosis
- Tonsillar hypertrophy
- Recurrent otitis media
- Sleep disturbances or apnea
An Overview Of GERD
When a person gets acid reflux or even heartburn, it is completely normal since it does happen to anyone at some point in their lives. However, they develop GERD when they experience these gastric symptoms more than twice a week. GERD, as research shows, is a condition where stomach acid flows back and forth, irritating the esophageal tube. This is due to the esophageal sphincter not closing correctly as the food enters the stomach and the acid backwash leaves a sour taste in the throat and mouth.
GERD & The Role Of Stomach Acid
The stomach acid in the gut system ensures that the consumed food is digested and transported to the intestines (both large and small) to be distributed to the body, making it function properly. Research studies have found that weak stomach acid and bile in the stomach can cause unwanted gut disorders like GERD, esophagitis, and Barrett’s esophagitis. When GERD is disrupting the stomach acids by forcing them to go back and forth in the esophageal tube, it can cause unwanted symptoms that can cause a person discomfort. Weak stomach acid can also trigger persistent symptoms causing it to be the key to reflux symptoms in the gut.
GERD & Asthma
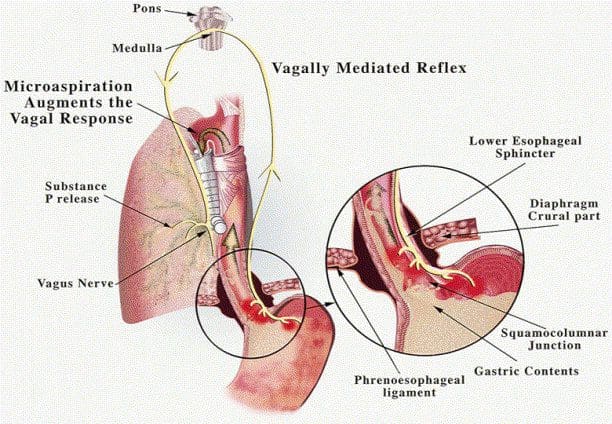
There are about 25 million individuals that have asthma, and this disorder can affect how a person breathes. However, GERD can trigger asthma symptoms by affecting the vagal reflex, the presence of acid in the esophagus, and the microaspiration of gastric contents into the trachea. Research studies have found that asthma and GERD can often occur together as GERD can worsen asthma symptoms. Conversely, asthma may cause GERD by altering the intrathoracic pressure, triggering the vagal reflex.
Other research studies have found that asthma causes chronic inflammation of the airways. When GERD interacts with asthma, it can cause an effect on the airways with an aspiration-induced response or even cause neurogenically induced inflammation. Since GERD is common for individuals with asthma, the symptoms and triggers can be developed into chronic issues over time. Studies have found that the installation of acid to reflux in the esophagus can stimulate vagal time and may trigger asthma symptoms in the airways.
Dilated Intercellular Spaces (DIS)
DIS or dilated intercellular spaces are also known as “leaky esophagus syndrome” as they are present on esophageal biopsy in virtually all GERD patients. Research studies have shown that DIS is considered a marker for GERD as the epithelial barrier is being reflected as an increase in paracellular permeability. The pathophysiology for DIS is thought to be repeated mucosal exposure to:
- Refluxed acid
- Digestive enzymes
- Bile acids
Dilated intercellular spaces may be responsible for the enhanced perception of proximal acid reflux and the symptoms in NERD individuals irrespective of esophageal acid exposure. Other research studies have shown that even though DIS is a structural marker of GERD symptoms, it does play a vital role in the pathophysiology of NERD individuals. DIS is also present in about 30% of asymptomatic patients with esophageal candidiasis, food allergies, eosinophilic esophagitis, and esophageal cancer.
Conclusion
Therefore, the gut system needs acid in the stomach as it helps break down the food into particles and be digested in the intestines, where it is transported throughout the entire body. When gut issues like GERD start to affect the wall linings of the esophagus, it can cause acid reflux and other symptoms to cause the gut to be upset. Suppose the symptoms are not treated right away. It can cause other chronic issues to flare up, like asthma symptoms and other gut disorders, developing over time, causing the body to be dysfunctional. Treatments for gut issues that are anti-inflammatory can provide relief to gut inflammation. They can even dampen the effects of inflammation not just in the gut but also in the entire body.
References
Ates, Fehmi, and Michael F Vaezi. “Insight into the Relationship between Gastroesophageal Reflux Disease and Asthma.” Gastroenterology & Hepatology, Millennium Medical Publishing, Nov. 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5395714/.
Badillo, Raul, and Dawn Francis. “Diagnosis and Treatment of Gastroesophageal Reflux Disease.” World Journal of Gastrointestinal Pharmacology and Therapeutics, Baishideng Publishing Group Inc, 6 Aug. 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4133436/.
Caviglia, Renato, et al. “Dilated Intercellular Spaces of Esophageal Epithelium in Nonerosive Reflux Disease Patients with Physiological Esophageal Acid Exposure.” The American Journal of Gastroenterology, U.S. National Library of Medicine, Mar. 2005, https://pubmed.ncbi.nlm.nih.gov/15743349.
Clarrett, Danisa M, and Christine Hachem. “Gastroesophageal Reflux Disease (GERD).” Missouri Medicine, Journal of the Missouri State Medical Association, 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6140167/.
Li, James T C. “Asthma and Acid Reflux: Are They Linked?” Mayo Clinic, Mayo Foundation for Medical Education and Research, 30 Mar. 2021, https://www.mayoclinic.org/diseases-conditions/asthma/expert-answers/asthma-and-acid-reflux/faq-20057993.
Mastronarde, John G. “Is There a Relationship between Gerd and Asthma?” Gastroenterology & Hepatology, Millennium Medical Publishing, June 2012, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3424477/.
Medical Professionals, Cleveland Clinic. “Gerd (Chronic Acid Reflux): Symptoms, Treatment, & Causes.” Cleveland Clinic, 6 Dec. 2019, https://my.clevelandclinic.org/health/diseases/17019-gerd-or-acid-reflux-or-heartburn-overview.
Orlando, Lori A, and Roy C Orlando. “Dilated Intercellular Spaces as a Marker of Gerd.” Current Gastroenterology Reports, U.S. National Library of Medicine, June 2009, https://pubmed.ncbi.nlm.nih.gov/19463218/.
Richter, Joel E. “Role of the Gastric Refluxate in Gastroesophageal Reflux Disease: Acid, Weak Acid and Bile.” The American Journal of the Medical Sciences, U.S. National Library of Medicine, Aug. 2009, https://pubmed.ncbi.nlm.nih.gov/19590427/.
Staff, Mayo Clinic. “Gastroesophageal Reflux Disease (GERD).” Mayo Clinic, Mayo Foundation for Medical Education and Research, 22 May 2020, https://www.mayoclinic.org/diseases-conditions/gerd/symptoms-causes/syc-20361940.
Disclaimer
General Disclaimer
Professional Scope of Practice *
The information herein on "GERD & The Role Of Stomach Acid" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multistate
Multistate Compact RN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics